This article is copied from PatientPlus, UK
Retinopathy of Prematurity (Retrolental Fibroplasia)
The retina is unique among developing embryonic and foetal tissues in that it has no blood vessels until the fourth month of gestation. The vessels grow out from the optic disc, only fully reaching the periphery of the eye one month after birth.It is the incompletely vascularised retina that is susceptible to oxygen damage, especially in the pre-term infant. Retinopathy of prematurity (ROP) is a proliferative disorder of this immature retinal vasculature. It ranges from being mild with no visual sequelae to severe with marked visual impairment or blindness. The exact pathophysiology is not fully understood and it is unclear why some infants develop it whilst others, in a very similar clinical situation, do not. It is one of the few mostly preventable causes of childhood visual impairment in this country.
ROP develops in 16% of all premature births, the figure rising to over 65% of infants weighing less than 1250gms at birth. Some studies suggest that as smaller and younger babies are surviving, its incidence is increasing. However, better understanding of screening and management of these babies has resulted, others say, in a decrease in its incidence. Risk factors are:
- Prematurity (particularly less than 32 weeks of gestational age)
- Low birth weight (≤1500gms and particularly if ≤1250gms)
- Oxygen therapy (hypoxaemia and hypercarbia also increase the risk)
- Co-morbidity
Development and progression of ROP relates to the baby's post-menstrual age - PMA (i.e. number of weeks of age since conception).The timing of screening and therefore the window of opportunity for treatment depends on this rather than the baby's post-birth age, especially in the more pre-term infants. The current guidelines are to screen all infants born less than 32 weeks of gestational age or weighing less than 1501gms. Babies born before 27 weeks are screened at 30-31 weeks PMA, babies born between 27 and 32 weeks or weighing less than 1501gms at 28-35 days post-natal age. Screening is weekly or fortnightly according to clinical findings and is carried out by ophthalmologists with a specialist interest in these problems. ROP does not occur until after vascularisation is complete and therefore babies who have not developed any problems by 37 weeks PMA need no further screening.
Screening: what does it involve?
|
Any systemic problems are related to prematurity rather than to ROP per se. Ocular consequences are described in 'complications', below.
There are a number of descriptors used to characterise the amount of ROP. Management and prognosis depends in the location, the extent, the staging and additional factors:
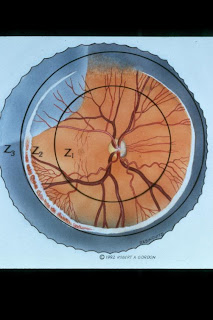
- Location: where it is - for the sake of description, the retina is divided into concentric zones centred around the optic disc. There are three of these, zone 1 being the innermost and zone 3 the outermost.
- Extent: amount of disease - the retina is also arbitrarily divided into clock hours and involvement is expressed in number of clock hours affected.
- Staging: what is occurring. There are several progressive stages, each describing increasing severity of the disease. They are:
- Stage 0 - no clear demarcation line between the developing but as yet non-vascularised area and the vascularised area.
- Stage 1 - a demarcation line appears between non-vascularised and vascularised areas.
- Stage 2 - the demarcation line becomes raised into a ridge
- Stage 3 - abnormal neovascularisation now occurs
- Stage 4 - the abnormal area detaches (retinal detachment)
- Stage 5 - stage 4 progresses to total retinal detachment
- Other factors - 'plus disease' describes features suggesting a tendency for ROP to progress:
- Gross vascular engorgement of the iris and the pupils fail to dilate
- Development of a vitreous haze
- Dilated and tortuous fundal vessels
- Vitreous and preretinal haemorrhages
For instance, a baby might be said to have ROP in 5 clock hours (12-5) of stage 3 disease in zones 2 and 3 in the presence of 'plus disease'.
The decision to treat is complex and based on the above characterisation of the ROP. Stages 1 and 2 need no treatment but stage 3 marks the point where treatment may be needed depending on extent and location. There are also issues surrounding the exact timing of treatment for it to be optimal. Once the treatment threshold has been identified, treatment needs to be carried out within 48 hours. Treatment options for stage 3 disease include laser therapy (first choice) or cryotherapy under general anaesthesia. A response should be seen between 2 and 6 days. Re-treatment may be carried out 10-14 days later if there has been a poor response. Treatment of stages 4 and 5 is more controversial as vitreo-retinal surgery may achieve reattachment of the retina but the visual outcome tends to be poor. Treatment tends to be to both eyes as the severity and progression of ROP in the eyes of a given baby tends to be similar.
Complications
Complications of treatment
Although treatment of severe ROP is associated with better long-term visual and structural outcomes, it carries a risk of both short- and long-term ophthalmic morbidities. These include:
- Uveitis
- Intraocular haemorrhage
- Conjunctival lacerations
- Vitreous, retinal or macular detachment
- Corneal haze
- Hypotony and occasionally, angle-closure glaucoma
- Cataract formation
- Myopia
- Iris atrophy
- Nystagmus
Cicatricial ROP
About 20% of babies with ROP go on to develop cicatricial complications which tend to be worse with more advanced and more posterior original ROP. There are 5 described stages:
- Stage 1 - myopia
- Stage 2 - vitreoretinal fibrosis which can pull on the retina
- Stage 3 - Severe peripheral retinal fibrosis
- Stage 4 - Partial retinal detachment
- Stage 5 - Complete retinal detachment ± secondary angle-closure glaucoma
- Stages 1 and 2 - the pathology completely regress back to normality with a good visual outcome for the child.
- Stage 3 - this is a turning point: the disease may or may not progress and it is these patients who need particularly close monitoring ± ablation of the abnormal neovascularisation to prevent going on to detachment.
- Stages 4 and 5 inevitably progress and require surgical intervention although there is not necessarily a good visual outcome, making this treatment controversial.
- Severe disease is relatively infrequent; one study found that only 18% of babies weighing <1251gms>
- ROP is more often associated with an increased risk of less serious ophthalmic problems associated with prematurity such as strabismus and myopia.

0 Readers' Says:
Post a Comment